I recently had the great pleasure of presenting for the New Jersey Society of Optometric Physicians (NJSOP) with a man who has become an optometric legend to me: Dr. Leonard Press (PressVision). After hearing and reading about my keynote speech at NORA in April, Dr. Press extended an invitation to speak with him for the NJSOP, and I was honored and excited to accept.
For several months, Dr. Press and I were passing emails back and forth. We finally met in person the night before our presentation and I immediately connected with him. He was warm, charismatic, and observant. For example, he immediately noticed what most people tend not to… that when he sat down to my left, I adjusted my posture to look at him straight-on instead of gazing in that direction, and he asked me about this.
As I have written about in a previous post, I have diplopia (Double Vision). The image that I see with my right eye is lower than the image that I see with my left, which I wear lenses to “correct” in a neutral gaze. One of my cranial nerves (IV) has become partially paralyzed since my severe traumatic brain injury in 2011. This causes the amount of my diplopia to be variable depending on the direction of gaze. For this reason, even with my glasses, I still see double in my left field of vision as well as when I look up. Dr. Press picked up on this immediately.
“You can rehabilitate vision the same way you do physical therapy, occupational therapy, and speech language pathology.”
Sitting together at the Bally’s Casino, Dr. Press and I had the time to discuss everything from medicine, to vision therapy, to brain plasticity and neurorehabilitation. I felt like I used to feel when playing in bands, and my band was about to open for a huge influence for us. This time, however, I was in emails with the headliner, and got to spend several hours with him both before and after the show! Over email, we agreed to format our presentation so that I would give mine first, he following right behind.
When brilliant people like Dr. Press speak, I listen attentively, especially when presenting about brain injury and rehabilitation. Dr. Press coauthored the go-to textbook from an optometric perspective, “Vision Rehabilitation: Multidisciplinary Care of the Patient Following Brain Injury.” A lot of valuable information was discussed between the two of us before and after our presentation, but I’d like to focus on Dr. Press’ portion of our presentation together: “Optometric Diagnosis and Management of Acquired Brain Injury and Concussion.”
After I presented, Dr. Press began by announcing some resources for brain injury from the optometric perspective. The first of these resources is, of course, NORA, the Neuro-Optometric Rehabilitation Association. Additionally, the vision rehabilitation section of the American Optometric Association (AOA) provides a helpful resource manual for free on their website. Another excellent resource is the aforementioned textbook coauthored by Lisa Harvey and Penelope Suter, “Vision Rehabilitation: Multidisciplinary Care of the Patient Following Brain Injury.”
Dr. Press began with the terminology and meaning of acronyms such as Acquired Brain Injury (ABI), which is the general term for ANY injury to the brain. This not only includes damage caused by physical trauma (TBI), but injury due to strokes, tumor, disease, or any processes that negatively affect the brain. In my case, we can easily tell what the event was that lead to my neurological deficits, but many times symptoms may arise from other kinds of ABI where “the neurological event” may not be so obvious.
“In the case of boxers…” Dr. Press explained “the cumulative effect [on the brain] can be greater than someone knocked out their first time in the ring.” He continued about a youth soccer player who presented with visual tracking problems. Finding the causative event took some detective work. Weeks before, her soccer coach instructed the team to head a ball against a wall over and over again, and afterward, “it looked like everything was bouncing.” On that note, Dr. Press included, “Teen brains are not woodpeckers.”

Sports vision is a growing field, especially when it comes to the assessment of a player’s ability to continue playing or not. Many times, brain injury goes undiagnosed. An extreme example of this was the news that my mother was given, as I laid in a coma, only hours after falling 20ft and hitting my head twice: “The good news is that he does not have a brain injury,” the nurse told her.
As concussions are now being recognized as the brain injuries that they are, visual testing of brain function is being adopted as a “remove-from-play sideline concussion screening test.” This field side test is called the King–Devick Test. The test was developed in 1976 by Alan King, O.D. and Steven Devick, O.D. to assess saccadic performance as it relates to reading ability. Saccades are the movements of your eyes from point to point, which are controlled by the brain. The brain will decrease in either speed, accuracy, or both after a concussion. Today, of course, there is an app for that.
Dr. Press went on to explain other common conditions with traumatic brain injury, but, what I found especially interesting was when Dr. Press said that “brain injury has nothing to do with static acuity.” Static acuity refers to the ability to clearly see an object that is not moving. When we talk about 20/20 vision, we are referring to static acuity. Raising his hand to shape an “O.” “Brain injury has nothing to do with static acuity. Zero!” he exclaimed. “[but,] with tracking: big time.” Most visual charts test this, which is why many brain injury survivors may have 20/20 vision, but still have severe visual deficits.
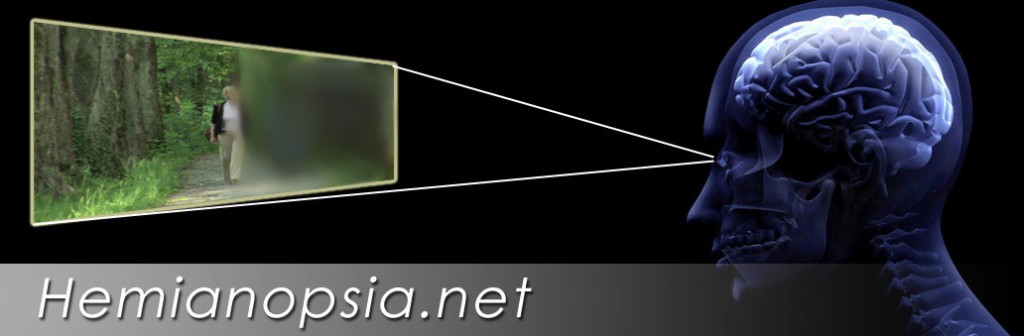
Probably the most common deficit in the family of TBI, is homonymous hemianopsia, or visual neglect. This is a visual field deficit in which one hemisphere of vision, either the right or the left, is “neglected,” or not recognized in both eyes. Hemianopsia.net is an excellent tool, not only for clinicians, but for patients as well. This condition eventually seems to get better, to some degree, with time, but with optometric intervention, recovery can be accelerated. Unfortunately, like my behavior surrounding some of my own shortcomings after my TBI, many patients do not realize that they have a problem. Again, how can one tell that it is raining when they are underwater?
A therapeutic tool that can help to address this condition is from TactusTherapy.com, which is actually a speech language pathology website. “Visual Attention Therapy helps people with visual neglect improve awareness of the neglected side of space.” Again, there’s an app for that.
Often we find helpful visual tools in several other practices of rehabilitation. As Dr. Press explained, the problem is that “in the rehab community, there isn’t good awareness that you can rehabilitate vision the same way you rehab with physical therapy, occupational therapy, and speech language pathology. So vision therapy is just as much, part and parcel, of the rehabilitation after brain injury as any other of the body systems.”
I wholeheartedly agree with this statement, even though, at one point in my recovery, I did not see VT as a priority. In working with many of those in the optometric community I know just how beneficial vision therapy can be for neurorehabilitation, and I can now personally attest to how instrumental it has been in my own recovery. I consider vision therapy to be one of the most important practices for me, and a practice that I continue to do every day.
I learned so much while presenting with Dr. Press at NJSOP, and it was an excellent reminder that there are many ways in which we can positively affect rehabilitation. I emphasize the synergistic benefits of different modalities and specialties that contribute to successful recovery, and I am pleased to play a part in championing vision therapy’s role in neurological rehabilitation.





6 Comments
Leave your reply.