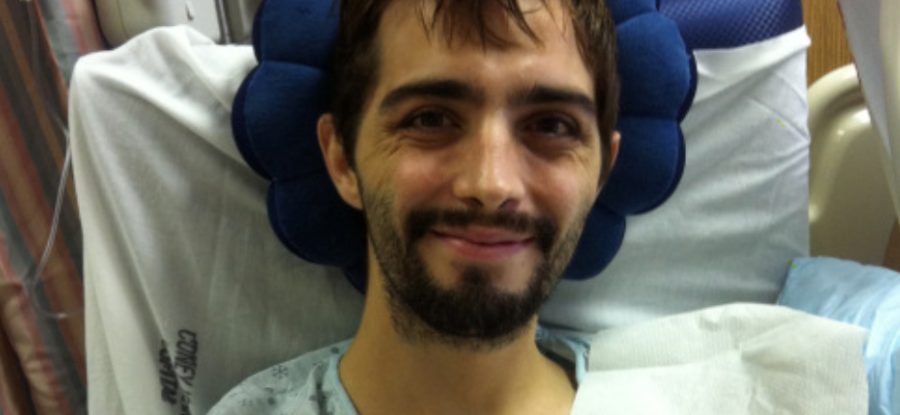
My next memory takes place during the day. My mother sat in a chair next to my inclined hospital bed. A pretty brunette in her mid-20s wheeled a cart carrying some sort of electronic equipment cabled to a computer monitor towards me. “Hi, Alicia.” My mother said warmly.
Although she had worked with me before, I had no memory of ever meeting her.
“Hi, Cavin. Welcome back.”
She sat by the side of the hospital bed and pressed a button that spun a motor to adjust the position of the bed to sit me more upright. I did not possess the strength to sit up on my own.
“Do you remember my name?” she asked. I stared at her blankly in sedated admiration. “I’m Alicia. I’m going to do a quick test. Is that ok?” I nodded. She placed a cup of ice chips on the tray by my bed and gently brought one to my lips. “Is that good?” she asked, and I again nodded.
As she put some sort of lubrication on one end of a long flexible fiber optic tube, Alicia began to explain that this tube was going to need to go through my nose. I don’t know how she did it, but my demeanor remained calm and cooperative despite the strange introduction of a foreign object into an unnatural orifice. As the tube slipped near what felt like my Adam’s apple, my weakened gag reflex mildly reacted to the irritation and my eyes began to water.
Alicia was performing a flexible endoscopic evaluation of swallowing (FEES) by feeding a fiberoptic camera through my sinuses and to the back of my throat. From here, the camera could see (scope) inside of (endo) my trachea. The monitor displayed the inner workings of my pharynx’ ability to swallow, or the inner workings of the valve that moves food from the mouth to the esophagus.
She slipped another ice chip in my mouth and asked me to swallow as hard as I could. My mouth and throat felt like they were coated with the desert sand of a dried up river, and the cool wetness of the ice was beyond refreshing. I let the cube melt in my mouth a bit longer and then I attempted to swallow, but it did not feel right… Nothing felt right.
The corner of Alicia’s mouth rose ever so slightly as she watched the bad news display on the monitor. Even my ability to swallow was undoubtedly weak. After a few more ice chips, she retracted the fiber optic camera while explaining that she wanted me to practice swallowing, one ice chip at a time. She handed the cup to my mom.
“His dyspraxia is even worse. He is silently aspirating.” Alicia told my mom softly. “Liquid is pooling on the valve that let’s food down one tube and air down the other.” She placed her hand where her chin and her neck met. “So liquid gathers on this valve, and then, when he breathes, the liquid ends up in his lungs… He is aspirating.” My mother was taking notes as Alicia explained. “Usually people cough whenever food or liquid ‘goes down the wrong tube,’ right?” She asked rhetorically, “Well, Cavin is not even coughing when he aspirates, and this is really dangerous because he is not even attempting to remove the food or drink that enters his lungs” she explained. “The lungs can handle a bit of clean water, but any food or drink other than water can lead to an infection in the lungs which could be life threatening.”
While in an induced coma, my ability to swallow had deteriorated even more. Dyspraxia is a general diagnosis of a difficulty swallowing, usually due to brain damage, and this condition had apparently worsened since the barium swallow test before I was put into a coma. Because my swallowing mechanism was not working properly, eating food orally posed a serious risk of aspiration, or of food going down the wrong tube and, into my lungs. And, because my cough reflex was also weak, when I aspirated, I would rarely even try to expel the food in my lungs. The poor communication between my brain and my swallowing mechanism (pharynx) posed a real danger. In order for me to receive nutrition, I was going to need to bypass this malfunctioning mechanism with an NG (or nasogastric) tube.
I don’t remember this tube being placed, but, like the path that the fiber optic endoscope had traveled, a feeding tube was inserted into my nose. It was fed through my sinuses to the junction of my esophagus and trachea (pharynx). At this point I was instructed to swallow the tube so that it would pass through my esophagus and into my stomach. The tube protruding from my nose was where I would be fed for months to come.
_____
Food is such an important aspect of our lives, and I know from my own experience that not being able to eat was maddening. There is a fine line to walk between rehabilitation and safety… we must keep foreign liquids and solids out of the lungs while also rehabilitating someone’s ability to swallow. It is very difficult for someone to recover when they are dependent on pureed food. Especially because typical gastric feeds are inflammatory processed liquid nutrition. Inflammation anywhere in the body contribute to inflammation to the brain, and the typical processed liquid nutrition is inflammatory.
When I work with clients, we are able to transition the gastric feed to one that is supportive to neurological function. This gives their brain the supplies needed to strengthen the pathways that give them the ability to swallow. We want to do the rehabilitation exercises while also supplying the nutrition.
If you find value in this post… or know someone else who may find value in it, feel free to share it. 💪🙏🤘




Leave a Reply
Your email is safe with us.