My old vision therapist just did an interview with my mother for his blog: VT Works! Take a look!
This post appears as part of a series called Sit Down – candid conversations with real people detailing their journeys and experiences with Vision Therapy.
A Sit Down – with Kris Balaster
For the benefit of our readers, can you explain how you are involved in Developmental Optometry?
My son Cavin fell 16-20 feet from a “water drum” scaffolding tower onto the rooftop of the building in Brooklyn, NY where it was installed. He was in the process of descending from the climb, when he slipped and lost his footing. Possibly during the fall he may have hit his throat on the underlying scaffolding. I am told by his friends that he landed on his feet for a brief moment and then fell backward onto the asphalt and hit his head. He was immediately unconscious and sounded like he was snoring. Someone in the group he was with had been an EMT and immediately called 911. The paramedics “bagged him” and rushed him to a Trauma Hospital in the next borough. He was measured at level 4 on the Glasgow Coma Scale at that point. There were not yet any signs of head trauma. He remained in a coma for 12 days. Because the initial CT scan showed no head injury, the neurologist couldn’t understand why he wouldn’t wake up and tried to shake him and yell loudly to arouse him to consciousness. There was no response. They even attempted to extubate him the next day, but he bit down on the tube and started thrashing. His oxygen levels de-saturated to 60% and so they abandoned the attempt. After that incident they noticed that he stopped moving his left side extremities (which had all been moving prior to this “attempt”).
A few days later they did an MRI and discovered that the reason he would not come to consciousness was because he had suffered Diffuse Axonal Injury [DAI] (also known as “shearing”). This is a situation caused by the forces from the brain being slammed forward and backward against the skull (also called “coup/contracoup”). This causes the dendrites (sheathes which connect neurons) to stretch and then swell. In response to this insult, the brain releases a chemical reaction known as a “calcium cascade” within the dendrites which destroy the axonal part of each neuron that is affected. Messages are transmitted from neuron to neuron through the axons and so this type of injury causes axonal death between those neurons and the patient loses those particular neuron’s previous functions. The neurologist just shrugged his shoulders and said that Cavin had extensive DAI throughout his corpus callosum (the middle part of the brain that acts as a switchboard between right and left hemispheres), and that he also had a subdural arachnoid hemorrhage and bleeding in his temporal lobe. It was a lot to take in. When I asked him what that all meant, he shrugged his shoulders and said “you get what you get”.
By that point, Cavin had developed pneumonia and MRSA (systemic staph infection) and was put on big gun antibiotics. Every morning when I arrived they would go through the laundry list of his injuries and tell me his current status. At one point I remember saying “but, he’s going to live isn’t he?” They said, “we don’t know”. I stopped asking.
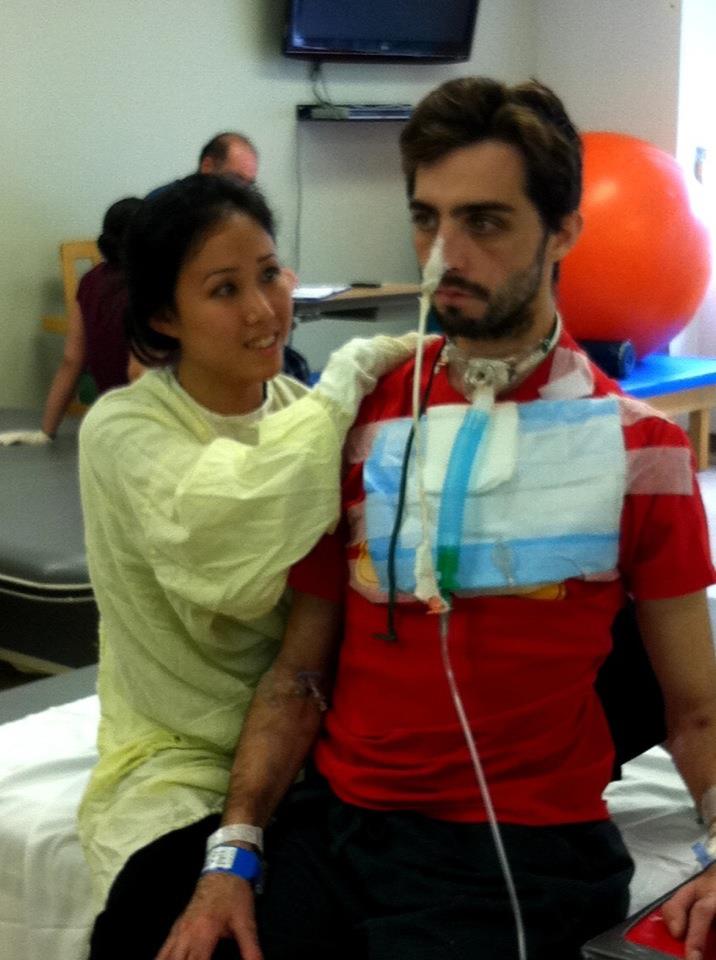
Once Cavin came to consciousness and was taken off life support, he was moved from Intensive Care to a “step down unit”. The social worker began making plans to transfer him to the Klingenstein Center for Brain Injury at Mount Sinai hospital. He remained on the step down unit for about 3 weeks. During that time he was cleared to eat pureed foods, so I was going to the hospital restaurant and buying high quality soups and pureeing them in a Magic Bullet blender. Then he started having breathing problems and they sent a Respiratory Therapist in to give him asthma treatments a few times a day. They would also give him Ativan, thinking that he was having panic attacks. One Friday night the Respiratory Therapist told me that he didn’t believe that Cavin was having asthma attacks. By Saturday morning Cavin told me that there was something very, very wrong. By Saturday evening he was using all his abdominal muscles to breathe and was so panicked that he was trying to crawl over the top of his bed. One of the doctors said she was going to call for a psychiatric consult as she suspected panic attacks. The head nurse kept calling for the attending physician because she knew something was very wrong. Remember, this was at a Trauma Hospital on a Saturday night in Queens, NY and the attending physician was downstairs in the ER and up to his neck in gunshot wounds, stabbings and other life threatening injuries. As Cavin worsened, the head nurse started panicking and continuing to call for help; the attending physician sent a resident up from the Emergency Room to check on him. The resident said that she was going to order a chest x-ray and bloodwork later that night or in the morning and that he didn’t seem to be in grave danger. The head nurse knew otherwise and called the attending physician again and told him that they were in grave danger of losing Cavin. The “attending” finally broke free and when he saw Cavin’s condition, he started demanding to know why he had not been informed of the gravity of his situation. He immediately called for an emergency intubation right there in Cavin’s room at midnight. He was then moved to Respiratory ICU where he was put into an induced coma for 7 days. I stayed until 3am that night to make sure he was stabilized and was then informed that I had to move everything out of Cavin’s room in the step down unit immediately. By that time a lot of “things” had accumulated in the room where he had just spent three weeks , so I starting filling shopping bags(7) with all his belongings and dragged them downstairs where security called me a “town car” which drove me back to my hotel with all these bags (of course it was also pouring rain)…. What a night.
His father took a “red eye” flight from Denver at 1 am and arrived at the hotel at about 6am. We both caught a couple hours of sleep and then went to Respiratory ICU. The doors were closed and the drapes were pulled around the bed but we could see 6 pairs of feet under the curtain and were told that there were serious problems that they were working on. We sat in the waiting room until they came for us. Apparently, the intubation was not done properly as they could hear sounds coming from his vocal cords in the ICU unit. As it turned out, they were extubating and re-intubating him as we arrived. This is a very dangerous procedure because it is not being done in an OR and if they lose their airway, they have to do an emergency tracheostomy which is better done in an OR. It was at that point that they discovered he had a stenosis in his trachea (scar tissue) that had reduced 3 centimeters of his trachea to the size of a drinking straw. They put him on steroids to see how much of the swelling they could reduce using that approach. The following Tuesday they took him for a CT scan of his throat and, quite to their surprise, they could see space between the breathing tube and his trachea. They decided to take him to the OR on Friday and extubate him there and scoped his throat to assess whether there was a stenosis. If so, they would do a tracheotomy.
We waited with baited breath for the results. The ENT finally appeared and said that there was no signs of stenosis, that he just had a “raw, ratty looking” trachea. He was discharged to another step down unit where he was assessed for swallowing and it was discovered that he was aspirating anything they gave him and so was put on feeding tube through his nose (an NG tube). He stayed for 10 days until we could get him transferred to Mt. Sinai.
Within 2 days of being at Mt. Sinai Brain Injury Center, his breathing problems returned. One of their top ENT’s assessed Cavin and saw that the stenosis was present and that it had only been masked by the steroids he had been put on at the other hospital. The Doctors were not happy about this, as acceptance into that Brain Injury Rehab is only for patients who are medically stable. A tracheostomy was scheduled for the next morning and the Surgeon told us that the stenosis was worse than he had anticipated. He had to bore right through the scar tissue to place the trach tube and didn’t know if Cavin would ever be able to live without it or regain his ability to swallow. His only option was for a tracheal resection later down the line and that he feared that too much of his trachea was scarred and they wouldn’t be able to repair it. This would also mean that he could never speak again because there wasn’t enough space to get air to his vocal cords. He said he’d take another look at him in about three weeks. I never told Cavin that. He was so disheartened and still being fed through the NG tube. He had lost 30 pounds, couldn’t walk, had no core strength to even sit up…. but he was cognitively intact enough to be really angry and hungry.
Things really changed after the tracheostomy. The very next morning Mt Sinai had him participating in the full program of neuro, physical, occupational, and speech therapy (mostly to work on his ability to swallow without aspirating the thickened, pureed food into his lungs).
He never did pass the swallowing assessment and so they had to place a feeding tube into his stomach. As the head physiatrist at Klingenstein told me “on this unit we’re in the business of taking tubes out of people, not putting them in”. He was not happy. Nobody was, believe me; especially Cavin.
In short order, his Occupational Therapist noticed that Cavin was closing one eye in order to be able to see. I didn’t fully grasp the cause or ramifications of his double vision, but I did notice that he was instinctively closing one eye in order to see and he had told me that when I got close to him, he saw four eyes. There were so many other pressing medical problems that I was trying to metabolize and work through with him that this seemed minor. The OT suggested that he wear an eye patch and switch it from one eye to the next so that he didn’t lose any visual acuity. I had just had his eyes examined the month before the accident and he had 20/20 vision. He was now using his IPhone and put it on a timer to alert him every 20 minutes, at which time he would switch the patch to the other eye.
When the ENT and his resident examined Cavin 3 weeks after the tracheostomy, I was in the bathroom of his room and didn’t hear them come in. They scoped his throat and told him that he was in better shape than they expected and “just” met the margins to be able to have his trachea re-sectioned (where they would cut out and remove the 3cm of scarred trachea and sew the “good ends” together). This is a very tricky and delicate procedure as the vocal cords can be damaged and the swallowing mechanism can also be damaged during the surgery. When I emerged from the bathroom Cavin wrote on his Ipad about what he had just been told. I burst into tears. He had no idea why. It was then that I told him the possible effects on his life from that undiagnosed stenosis which had been given 6 weeks to grow before being treated. We proceeded to schedule surgery and were told it might be a few months.
Cavin had run out of time at Mt. Sinai and the only option was to send him to a subacute nursing home or for me to find housing (or a hotel) where I could care for him until he got the surgery.
By this point he was using a walker for short distances, but still needed a wheelchair and humidified air to a tube leading to his trach to give him enough moisture to keep his respiratory system healthy. He was also on PEG tube feeding for nourishment.
I did manage to find an apartment where we moved for 2 ½ months. There, he received Visiting Nursing Services, including OT and PT and respiratory therapy monitoring (I had 6 large oxygen bottles, a tracheal humidifier that he was to be on, nebulizer and some kind of mixture that I administered twice a day, trach tube cleaning kits, PEG tube supplies, a shower seat, wheelchair, walker…. The whole 9 yards). He did have the tracheal resection surgery in August and stayed again in the hospital for about 4 days. The surgery was a complete success! He was finally able to talk again, but still needed to be assessed for swallowing. The Dr. who performed the resection had Cavin meet with his speech pathologist (who was leaving town the next day for a 2 week vacation). She cleared him enough to eat small amounts of pureed food, so I would cook and puree the bulk of his food and force it through a syringe into the PEG tube, and then give him a little cup of it to sip so he could have the taste of what was going into his stomach.
The head physiatrist had given me several prescriptions when we left, and one was for an appointment with the SUNY school of Optometry. In September, we were seen by Christy Sell OD, who did a comprehensive exam of Cavin. She was very thorough and found that Cavin had double vision (4th nerve palsy) and prescribed glasses with a 7 Fresnel “stick on” lens for him.
You have lived through every parent’s nightmare – a phone call in the middle of the night, Cavin hospitalized over 1700 miles away, vague details on the phone about his condition, and many unknowns even about his potential for his survival. Can you describe that initial 24 hours?
When I first got the call from Cavin’s father at 4:30am, he told me in a panicked voice that “Cavin fell”. I said what do you mean? He said he had just gotten a call from a policeman who told him that our son was in critical condition and on life support from a “fall” and that he had been trying to call the ER to get more information, but nobody would pick up the phone. He suggested that I try to call them…. I instinctively knew that our son was in grave danger and that there was no way that I was going to call anyone…. I was going there immediately. I kept pacing the floor screaming “NO! NO! NO!”, in between attempts to book the next flight to New York on the internet and throwing things into a suitcase. Though stunned, fearful, and bereft, I knew I needed to get there immediately. I booked a ticket and made it to the airport in Austin to catch a 7am flight and arrived at the hospital in New York by 1 pm. I was met by my other son and several of Cavin’s friends in the waiting room. They gave me the rundown of what and how it all happened. I went into see him and it was pretty hard to take in. I think I was just numb. I took his hand and stroked his head and told him what had happened, where he was, and that he had taken a bad fall. I also told him that there was going to be a long road for him to get better and that a lot of things would be changing day to day, but there would be one thing that was constant…. I would always be there and that I was going to walk him through this. I repeated this to him through every stage of his recovery. He squeezed my hand.
When you arrived in New York, what specific information were you given about Cavin’s condition?
I was told that he was comatose, on life support, had 6 broken ribs and 3 pelvic fractures as well as a lacerated kidney, but that he didn’t have a head injury according to the CT scan done that night. I remember the charge nurse saying “Thank God he doesn’t have a head injury…. That’s your Mother’s Day present (yes, it was Mother’s Day). As the days went by, it turned out that he had one of the most serious forms of head injury one can have.
All told, how long was Cavin in the hospital and can you describe his condition when he was released?
Cavin was hospitalized from May 8 until July 24, 2011. He was then hospitalized for another 4 days in August for the tracheal re-section operation. During this time I worked with his roommate to find another renter to take over his share of the lease, and had to do a lot of “mop up” from his former life, and then pack him out of there. He was in the sound equipment rental business so he had lots of large equipment that needed to be dealt with. Once he was walking with a cane he and I travelled to his apartment in Brooklyn and inventoried everything and then made arrangements to have all that equipment picked up and put on consignment. He had been living in New York for 8 years and, in addition to his sound rental gear, he had 5 guitars, amplifiers that he couldn’t part with, etc. He also had a dog which his new roommate “adopted” and cared for during that time. The dog stayed in New York, the rest of his stuff came back to Austin when my fiancé drove from Austin to New York and picked us up on October 2, 2011. We looked like the Beverly Hillbillies. The car was so packed that there was barely room for Cavin to sit. The process involved a lot of “letting go” and yet keeping enough of his former identity to stabilize his sense of self. Cavin was walking independently with a cane at this point, but had the gait of someone with Cerebal Palsy. His left arm was always “crooked out” to stabilize him. My best friend (who was present at his birth and referred to earlier) came to visit us in late October and was frankly surprised that he was doing as well as he was.
You and Cavin have both shared with me the struggles and turbulence that your mother/son relationship suffered as he began his recovery. This seems to be a common occurrence in families where a Traumatic Brain Injury has occurred. Can you describe how it affected your household?
I graduated from college with a Bachelor of Science Degree in Rehabilitation Education in the early 1980’s. From there I became an early childhood development specialist and worked “one on one” with infants and preschoolers who had been born with disabilities. I learned so much from that job. Following that, I studied and practiced psychoanalysis for many years. Psychoanalytic training requires an in-depth study of human psychological development from infancy through adulthood. I remember it occurring to me that I had spent most of my professional life studying for what was now happening in my life and the life of my son. It was kind of an eerie feeling, as though I had, on some level, been preparing for this moment my entire life. I began to feel very grateful for all that training, because I was “re-living” every developmental stage of childhood with him again, and, because I had already done so, I didn’t feel stymied by the regressions he went through. It was grounding for me to at least have a mental “Map” of human development and such intimate knowledge of raising him and could roll with the advances, plateaus and regressions that his progress was going to require. I was also very familiar with the stages of grief following a loss, and could get outside help for my stages, and provide guidance for his various stages of grief. Even though it broke my heart to see him come to realization and terms with his losses, I knew that it was necessary in order for him to heal. I sheltered him from those who were in complete denial, and I let him “try his wings” with those people I did trust. He wasn’t really comprehending “cause and effect” and the concept of time and schedule and we had quite a few “go arounds” concerning that. We also had hundreds of “late night talks” out on the patio. Sometimes I counseled him, and many times I let him counsel me. He “settled in” to his new life, and we were fortunate enough to have a “work from home” structure in which we were able to give him a “job” to do within our recruiting business that kept him challenged within a structure, but which also gave a lot of leeway for him to get plenty of nourishment and sleep that his brain desperately needed in order to heal. When he was able to work, he did an excellent job and contributed to the household income and this was very important to his self esteem. It also took some of the burden of my time away from the office (4 days a week) and my production levels. My fiancée was very supportive. Cavin’s days and nights were turned around and oftentimes we would awaken to the smell of him cooking at 4 am. His sleep patterns were very erratic, as were mine. I eventually realized and medically confirmed that I was in adrenal “burnout” and am still in the process of trying to heal myself.
One emotion that seems to be prevalent in all families where someone has suffered a Traumatic Brain Injury is that of denial. Did your family struggle with this?
(Chuckle) – In some ways I wish I were more blessed with the defense of denial. I am the kind of person that spots the repercussions of EVERYTHING and then the impact of EVERTHING ELSE that will be affected. For me it was a more a test of faith and acceptance than of denial. I remember, after about 4 days, going out to the Living Room where my ex-husband and I were staying at the time and falling to my knees sobbing my heart out. Cavin’s dad came out and asked “what’s wrong?” and I thought “What do you mean? Everything!!” I told him that we may have a seriously handicapped son on our hands for the rest of our lives. I was filled with terror and grief. I don’t think his dad would let himself “go there”. As Cavin got better, and was the “shining star” at rehab as I saw him in comparison to other patients, I felt like he was normal and pretty well on the way to recovery. Shortly before we left New York, he had a neuropsych evaluation at Mt. Sinai over a two day period. They normally would not even do such an evaluation for a patient so early after a brain injury (9 months minimum) and he was only one month medically stable, but he was doing so well that they decided to establish a baseline on him. I received that report about 2 days before we were left New York and felt stunned by the results. I had not come into full acceptance of how cognitively injured he was. I called my best friend and both read and cried to her about the results. I told her “my baby is really damaged”. She just said,” yes, I know”. I hated that feeling. But, as we got him to Austin and back within the “normal population” I could start to really start to comprehend and begin the acceptance process of how globally injured he was. That ended up being a blessing, because the phase following my own acceptance of that truth was to begin to understand that he, too, didn’t realize how injured he was, and to help him come to terms with it. There definitely were messages coming from his dad and that side of the family that he needed to “get back on the horse” and start riding again. Living with him in my home, I could see both sides; an incredible amount of drive, coupled with an tremendous amount of exhaustion. We were both exhausted beyond belief. He spent the next 18 months at my house. Initially, he wanted to pick up and return to his old lifestyle but in short order, he discovered that things were no longer the same. He writes about that it his blog on his website and says “how do you know it’s raining when you’re underwater?” I met a woman last year whose partner had suffered a TBI from a fall from a ladder. She asked me when I knew I could “let go”…. as in “leave him alone in the house” or determine how safe he was in situations that required independence and good judgment.
I told her that from my experience, it was not until Cavin was as fearful of his own safety as I was that I knew he was ready to move to more independence. The statistics say that someone who has suffered one brain injury is 50% more likely to suffer a second one. After a second injury, the percentage jumps to 80% for a third brain injury. Cavin initially felt that all he needed was an apartment and a car when I brought him to Austin. He talked about wanting to skateboard again and drive etc. In retrospect he realizes that he was in a total “brain fog”.
Following Cavin’s release from the hospital, how did you discover Vision Therapy and why were you looking?
When we left New York, we no longer had a “map” for his rehabilitation. At Mt. Sinai, as long as he was in their system, they just told us what to do next. I had limited funds and decided that the most important therapies, short term, were physical, speech, and vision therapy. He had diploplia (double vision) and severe dysaurthria (slurred speech), in addition to his ataxia (poor coordination on his left side) and balance problems. There was an aquatic center nearby my house that had a staff of physical therapists. An aquatic environment to stabilize his balance seemed like a perfect fit. We started there.
We also started yoga, which I had been doing prior to his accident. The owner of the studio was so kind and gracious and she accommodated Cavin’s needs and even set aside a special private session for him to come up with adaptations to the various yoga positions.
When he was interviewed here, Cavin wrote that he was in Vision Therapy for close to two years with Dr. Smith. From your perspective, how did it help?
My instincts were telling me that Cavin was losing ground in his visual perception. I searched and searched for an optometrist to treat a TBI patient with double vision. I finally found Dr. Denise Smith. We set an appointment and it turned out that Dr. Smith had done her residency at SUNY optometry with Christy Sell (from earlier section of this blog). It turned out that Cavin’ vision situation was fragile and had lost a lot of ground in the 12 weeks since he had been prescribed the #7 Fresnel Prism. I signed him up for several weeks of vision therapy and re-evaluations. I will never forget leaving Dr. Smith’s office that day. She teared up and said “thank you for doing this for him”. I was stunned and deeply touch by her statement. She went on to say that “most people don’t realize how important this is in treating a brain injury”. We paid out of pocket for several months until Texas Department of Rehab Services accepted her clinic as a “DARS” provider. At her clinic, they were able to determine that Cavin’s primitive reflexes (Morro) were overriding his more advanced reflexes. They went back to basics and advanced him to develop more mature reflexes. Even though he had regressed to needing a #9 Fresnel Prism by the time Dr Smith evaluated him, we kept him at a #7, started vision therapy immediately, and he progressed quickly back to a #7, then #6, #5 and ultimately to a #4 Fresnel Prism. I was taught by Dr Smith and her vision therapists that the eyes “look” but the brain “sees”, and that the brain would take the path of least resistance. They also taught me that it was crucial to train the brain to meet the demands of the “optic” world and not succumb to its “path of least resistance”.
One thing that has continued to fascinate me about Cavin is although he still has limitations, he is not one to seek pity. Instead, he has turned his misfortune into an opportunity to educate others. As his mother, where do you see his motivation coming from?
Cavin has always been a very creative person. He has always loved life and life has always loved him. I do believe that the stability was essential. My time in New York, being at his side daily was critical to his sense of security. At times, he would text me in the middle of the night screaming “help me mama!!!!!” I would call the nurse’s station and ask them to check on him. He was suffering from extreme paranoia and believing that he had been kidnapped by aliens. I knew that I needed to reassure him that I was in touch with the nursing station and would be there in the morning. He remembers nothing of these episodes. I didn’t take it lightly, I was very distressed as well. At this point I’ll tell you a funny (not so funny) story. When Cavin was about 9 years old we took the family to Alaska. His father decided that it would be a good idea to hike onto a glacier. We rented bikes and proceeded up the trail towards the glacier. It became apparent to me that we had gone beyond the trail, so we ditched the bikes and started hiking. We had a “bear encounter” in which she (thankfully) let us go, but we had to traverse several hundred feet of ice covered granite to get to the glacier. Once we did that, Cavin started to think we were in Disney World. There were 400 foot crevasses within that glacier and he didn’t fully comprehend the level of danger we were in. The more I tried to explain it to him, the more cavalier he got. I finally realized that the only way to “reel him in” was for me to get terrified and enlist him to help me get down from the glacier. It became a parallel situation during his TBI. I needed, at times, to put him in charge of my well-being. I have found this to be a very appropriate and empowering strategy. The TBI survivor is not the only survivor. The loved ones also need help.
Lights, Coma, Action is the title of a book Cavin is writing which will detail his accident, hospital stay, and subsequent recovery efforts. I know many of us in Developmental Optometry are very excited to share in Cavin’s story. How do you feel his book will be received?
It is my hope that Cavin is able to reach survivors and their families about the trajectory of TBI recovery and both manage their expectations, as well as provide real solutions to the challenge of TBI recovery. When I consulted with neuropsychologists in Austin, they told me that the body healed within one year. There was a two year window for the brain to heal. While they didn’t state that after two years, we were going to see the most progress he would ever make, they did say that the progress would plateau.
Following his interview on this blog, the Developmental Optometry community really stepped up to help Cavin reach his goal in fundraising, which was a phenomenal showing of support. Can you describe how you felt when you learned he had hit the mark and his book was to be funded?
I had no idea that Cavin was about to launch a Kickstarter program. He’d been talking about it for months, but I didn’t know he was about to “go live”. We had just gotten back from a major trip to Portland, Oregon for a conference on functional medicine, and the next thing I knew, he informed me that he had launched a Kickstarter to raise $15,000 in one month. I was terrified, frankly, because I feared that if he failed that he would question his whole “raison d’etre”. But, if you know anything about Cavin, he is a very passionate and determined person. I also knew that he needed a broad platform of support. Cavin has done so many wonderful things for people in his life, and they all really showed up for him during this campaign in whatever ways they could. Your blog interview took things to a whole other level. It was so amazing to see the response from the Developmental Optometry community. I can’t even begin to tell you how empowering that kind of support was. He really got confirmation that he has something valuable to contribute to Brain Injury Survivors and also solidified in his mind how the progress he made through Vision Therapy was so crucial to his “holistic” progress in recovery.
Your blog was such a gracious and wonderful event in our lives. I can’t thank you enough.
Cavin has, in many ways, turned his misfortunes into great positives as he works hard to educate others on the effects of Traumatic Brain Injuries. This includes being named the keynote speaker at the NORA conference coming up in April in Cary, North Carolina – quite a leap from that hospital bed some three years ago. How do you feel about these developments?
One day when we were driving back home from one of his therapies, Cavin said to me, “you know mom, I know that my TBI closed a lot of doors for me, and frankly, some of them needed to be closed. But it also opened doors for me. I now have a better feel for my work here on Earth. Before I was just “doin’ my thing” and that could have stretched on for years with nothing really accomplished. This really hit the reset button on my life”. I remember tearing up at those words, because, as a mother, you’re processing the thought of “what should have been”, etc. What has been so amazing to me is how he has been willing to expose the most vulnerable moments (on You Tube with Baby’s First Steps, on his blog, etc.). The response from the VT community was so heartwarming and confirming that he was on the right path and that he had so much to contribute.
Your message, your perspective, and your input are equally powerful in helping families navigate the waters which you and your family have been through. A few months back, we discussed the idea of your writing a book offering ideas for families where a brain injury has occurred. Do you feel like you’ll ever be ready to take on that challenge?
I spent the first 18 months securing therapies and taking him to them. Once we were out of New York, he no longer had insurance. We were now “on our own” to create a map. Thankfully the Texas Department of Rehabilitative Services had a program for TBI and Spinal Cord Injuries which allowed for 130 hours of therapy. But, we had to go through an administrative process and be put on a waiting list which could take up to 4-5 months. We didn’t have 4-5 months to wait for therapy to begin, because I could already see him losing ground.
My sister is a functional medicine practitioner in Houston and had recently been to a conference where she met another doctor and told her about Cavin’s accident. This doctor said that if she had a son in that condition that there was one person she would take him to. Unfortunately, she explained, this doctor resided in Austin. My sister exclaimed, “That’s where my nephew now lives”. We contacted him and put Cavin under his care immediately. He is a “functional neurologist” who was able to change the course of Cavin’s recovery.
Cavin has been so prolific in his writing about all the things that he did to heal himself that I’m not sure that there would be any material that I could add. However, I do long for a creative outlet and hope that someday I will have the time and space, and will have “settled down” enough from my own emotions to really think about what might be valuable to write about concerning this topic.
Lastly, many people who read this interview may be in the same position you were three years ago when your phone rang. What advice can you offer them?
First I would encourage anyone who has unmarried sons or daughters over the age of 18 to have a discussion with them and have them sign and notarize a Power of Attorney and Health Care Proxy Form to their parent(s) or someone they trust. Because I did not have that, I ran into so many problems for 6 weeks until Cavin was able to be cognitive and evaluated by a psychologist to verify that he understood what he was signing. I could not get access to the items they put into a vault after his accident (his wallet and therefore identification, his iPhone, his bank cards, bank accounts etc.). Luckily once I got his cell phone and his roommate told me his password to his bank accounts I was able to at least transfer money into those accounts (he did everything electronically so there were no statements to get account numbers for or from), and the banks reversed the fees charged for the overdrafts incurred by his (and my) inability to transfer funds between accounts. I have encouraged several of my friends to do this and they have been very appreciative of that information.
Secondly, depending on your personal circumstances, make sure you put the oxygen mask on yourself. This journey is the “long game”. I went to New York for 5 months, for the most part, alone. One of Cavin’s friends joined me the next day at my hotel for 4 days and told me that I was sobbing in my sleep. I have always had issues with anxiety but was always “ anti-psychotropic” medication. I was able to make an appointment with a psychiatrist through connections I had in Colorado and he prescribed me the perfect medication to keep me functional yet “take the edge off” the intense anxiety and pressure I felt. I was definitely in it for the long game. I saw this Dr. every week for a few weeks and then every other week and then once a month during my stay in New York. God Bless good Psychiatrists.
Thirdly, I would encourage people to really get in touch with their CORE VALUES and CORE BELIEFS. I told Cavin’s friends that I didn’t blame any of them for the accident and that I knew that they loved and cared about him. I spent many days and nights at the hospital repeating the Mantra “Thy will be done”. I decided almost immediately that I was not going to judge the situation…. And I worked towards surrendering to acceptance that this was part of Cavin’s and my journey in this life.
Some Closing Thoughts – A very special thank you to my friend Kris for taking the time for this interview. Understandably, answering these questions took incredible strength and courage and I am so grateful that she agreed to do it. I first met Kris the weekend after Cavin’s interview posted back in October, and what was supposed to be an hour lunch, turned into a close to five hour visit as she and Cavin shared their respective stories. Luckily for Cavin, his mom is one of the strongest women alive. Her determination to help her son and her will to find what was best for him truly is monumental, and a great role model for Cavin to follow. Please join me in thanking Kris for sharing, and in wishing her the absolute best! 🙂








4 Comments
Leave your reply.